How to make a basic dressing in a low-resource setting: instruction manual
1 Jul 2024
How to make a basic dressing in a low-resource setting: instruction manual
Authors: Jadesola Akinwuntan [1,2], L. Claire Fuller [3,4], Eric Comte [5], Hubert Vuagnat [6]
- University of Kansas School of Medicine, Kansas City, KS, USA.
- Massachusetts General Hospital, Boston, MA, USA.
- London Bridge Hospital, London, UK.
- International Foundation for Dermatology, London, UK.
- Geneva Health Forum, Institute of Global Health, Geneva University, Geneva, Switzerland.
- Wound Program, Healthcare Directorate, Geneva University Hospitals, Geneva, Switzerland.
Conflict of interest: None
Key words: Wound; dressing; low-resource setting
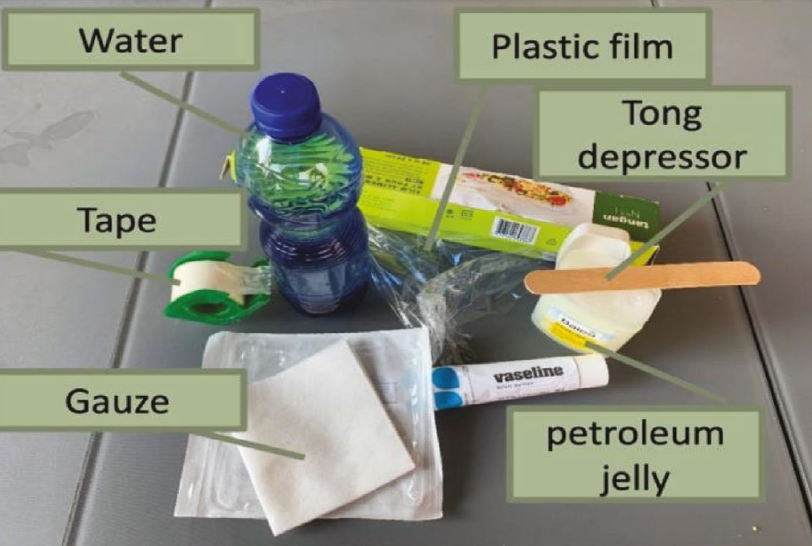
Materials needed (See Fig. 1.)
- Soap.
- Clean water (boiled or heated to over 70 oC and allowed to cool).
- Hydroalcoholic solution like hand sanitizer (optional).
- Greasy, moisturizing agent such as petroleum jelly, shea butter, palm oil, coconut oil, olive oil or another moisturizing oil.
- Gauze squares, nonwoven gauze is preferred.
- Tape.
- Plastic film.
- Bandages.
- Waste bag.
Instructions
- First wash hands with soap and clean water or hydroalcoholic solution.
- Prepare necessary materials.
- Wash hands with soap and clean water or hydroalcoholic solution before removing the old dressing.
- If the dressing sticks, use potable water to remove it. To take off the bandage and sticky tape, pour water or saline over and between the skin and dressing and allow time for the water to soak in. Lift and pull gently from periphery to the centre. Try to peel off, without pain or trauma and use as much water as needed to achieve this.
- Gently clean the wound and surrounding skin with potable water.
- Soap can be used if wound is very dirty but remember that it can irritate the skin.
- Avoid causing trauma to the wound when cleaning. - Rinse wound and surrounding skin with saline (NaCl 0.9%) if available.
- Gently dry the skin surrounding the wound using a dabbing motion. (Do not rub.) Leaving humidity within the wound is not a problem.
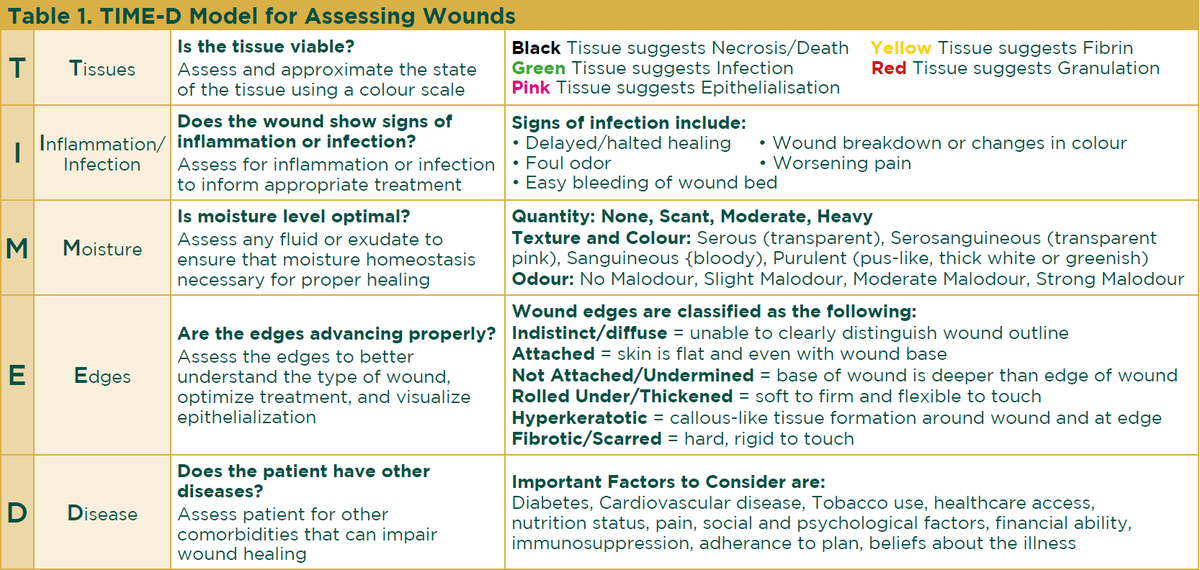
- At this point, use an instrument like the TIME-D model (Table 1) to assess the wound and plan for additional steps.
- If the skin is necrotic (black) or has fibrin (yellow), you will need to do an instrumental debridement. - Wash hands with soap and clean water or hydroalcoholic solution before making the new dressing.
- To protect the skin around the wound, gently spread a greasy agent such as Vaseline®, petroleum jelly, shea butter or palm oil over it.
- Always touch the greasy agent with clean gloves or clean tools if taking it out of a pot. Never go back a second or third time with the same glove/tool, to prevent contamination. - Gently spread the greasy moisturizer on some gauze to cover the approximate size of the wound. Place the greasy gauze interface onto the wound. This is the primary dressing, and as a contact layer it must not stick to the wound.
- Apply a second layer of gauze (without a greasing agent) over the first layer of gauze to help absorb exudate; this is the secondary dressing. It can also help to protect from external trauma. The second gauze layer should be roughly unfolded and bunched or ‘fluffed’, to look like a bridal veil, rather than neatly folded (see Figure 2).
- If there is too much exudate or excess fluid, add additional gauze layer(s) or a high absorbent dressing to absorb excess fluid. - Apply plastic film that is slightly bigger than the gauze, on top of the gauze layers to prevent moisture loss and diminish bacterial contamination; this is the tertiary dressing.
- Apply tape all around the edges of the plastic film to secure gauze and plastic film in place. Avoid heavy-sticking tapes to prevent mechanical damage of the skin when the tape is removed in the future.
- Wrap the area in bandages to help secure the dressing in place and offer a final protective barrier. Make sure the bandages are bigger than the wound area so everything can be covered.
- Unless the patient has a peripheral arteriopathy (i.e. impaired arterial supply as evidenced by weak or absent peripheral pulses), all wounds benefit from compression, so use the elastic bandage to provide it, starting distally and working proximally up a limb, in a circular and ascending manner, with greater pressure below than above to allow drainage. Each turn of the bandage overlaps the previous by 2/3 of its width, leaving 1/3 uncovered. Check it is not TOO TIGHT – you should be able to put your finger between the wraps of the bandage.
- Throughout all the process, evaluate pain and give appropriate pain control, such as acetaminophen or paracetamol.
- Ideally, for noninfected wounds, dressings can be changed twice a week if they are not soaked through by exudate and do not stick at removal. If the wound is infected, it may require daily changes.
- Wash hands with soap and clean water or hydroalcoholic solution after finishing the new dressing.
20. Store clean items, dispose of waste properly and clean any instruments.
21. Wash hands with soap and clean water or hydroalcoholic solution.
24. Repeat these steps for dressing changes for as long as needed until new skin has formed over the wound bed.
25. Advise the patient to move at all times despite the bandage. If needed for wounds at or near a joint, provide instructions for exercises to maintain the joint’s mobility.
26. Once the skin is closed, it remains fragile, it must be protected from sun and mechanical forces (blows or shear forces). Use of an emollient (same greasy agent as in point 10) in a thin layer to hydrate it twice a day for at least a few months is optimal.
The information provided is not intended to be a substitute for professional medical advice, diagnosis or treatment. All information is to be adapted to the patient’s unique condition.