The six basic principles of wound management for low-resource settings
1 Jul 2024
The six basic principles of wound management for low-resource settings
Authors: Jadesola Akinwuntan [1,2], L. Claire Fuller [3,4], Eric Comte [5], Hubert Vuagnat [6]
- University of Kansas School of Medicine, Kansas City, KS, USA.
- Massachusetts General Hospital, Boston, MA, USA.
- London Bridge Hospital, London, UK.
- International Foundation for Dermatology, London, UK.
- Geneva Health Forum, Institute of Global Health, Geneva University, Geneva, Switzerland.
- Wound Program, Healthcare Directorate, Geneva University Hospitals, Geneva, Switzerland.
Abstract
Chronic wounds develop when there is a problem with the natural healing process, leading to prolonged or incomplete resolution. Although the global burden of chronic wounds is still not properly identified, this issue can lead to significant financial, social, physical and mental challenges. Proper wound healing techniques can help offset the devastating effects of chronic wounds in resource-limited settings. In addition to a lack of knowledge, one of the biggest barriers to proper wound care maintenance is the direct and indirect costs generated by the care. This article aims to briefly discuss normal wound healing, provide knowledge on the basic principles of wound healing, and provide information on how to make a simple, low-cost dressing in a resource-limited setting in order to promote skin repair. Healthcare providers at all levels of training and community members should be familiar with these notions to lessen the progression into chronic wounds and shorten care length.
Conflict of interest: None
Key words: Chronic wounds; wound healing; dressings; cost-efficiency; wound bed; ulcers; middle- and low-income.
Key learning points
- To discuss normal wound healing.
- To provide knowledge on the basic principles of wound healing.
- To provide a guide on how to make a simple, low-cost wound dressing in resource-limited settings.
Introduction
Although there is no official global data, chronic wounds are estimated to affect approximately 2% of the total population in in the USA.1 One hospital in South Africa found that 34.6% of their 518 patients in a single day had acute wounds.2 One major community-based cross-sectional study in India reported an overall prevalence of chronic wounds of 15.03 per 1000 of the population.3 Low-resource settings around the world, lack of proper wound care materials and trained personnel often lead to chronic wounds and high infection rates.2–5 The global costs for wound management in the UK alone are GBP £8.3 billion.6 There is limited epidemiological and financial data for low- and middle-income countries.2,3,7 Chronic wounds can also lead to chronic pain, decreased physical and social function, loss of productivity and disability.7 These effects can often be prevented with prompt and proper wound care. However, the limited resources for wound care in low-income countries remain a major barrier to successful wound healing.8,9
Basic skin anatomy and wound healing physiology
Many health caregivers are not familiar with the key principles surrounding the selection of wound dressings that are required for successful healing. Effective dressings are selected to recreate the body’s normal conditions, so understanding the basic anatomy of the skin and the wound healing processes is essential to inform the appropriate choices.
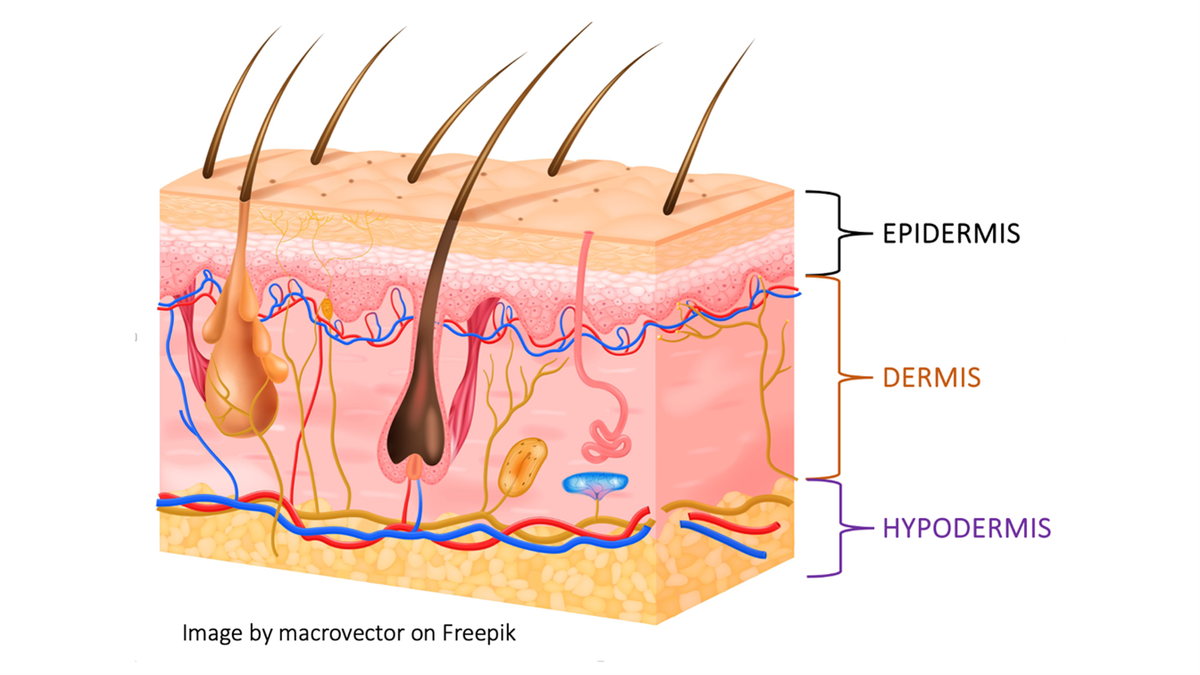
The skin consists of three layers – the protective outer layer called the epidermis, the supportive middle layer called the dermis and the fatty lower layer called the hypodermis (Fig. 1). The role of the skin is to act as a defensive barrier, to regulate body temperature, and to allow us to interact with our environment. A wound is essentially any form of damage to any of the skin’s layers. It can be caused by direct trauma such as burns, accidents and animal bites or by medical conditions such as dermatological diseases, venous insufficiency, infections and cancer.
The stages of wound healing
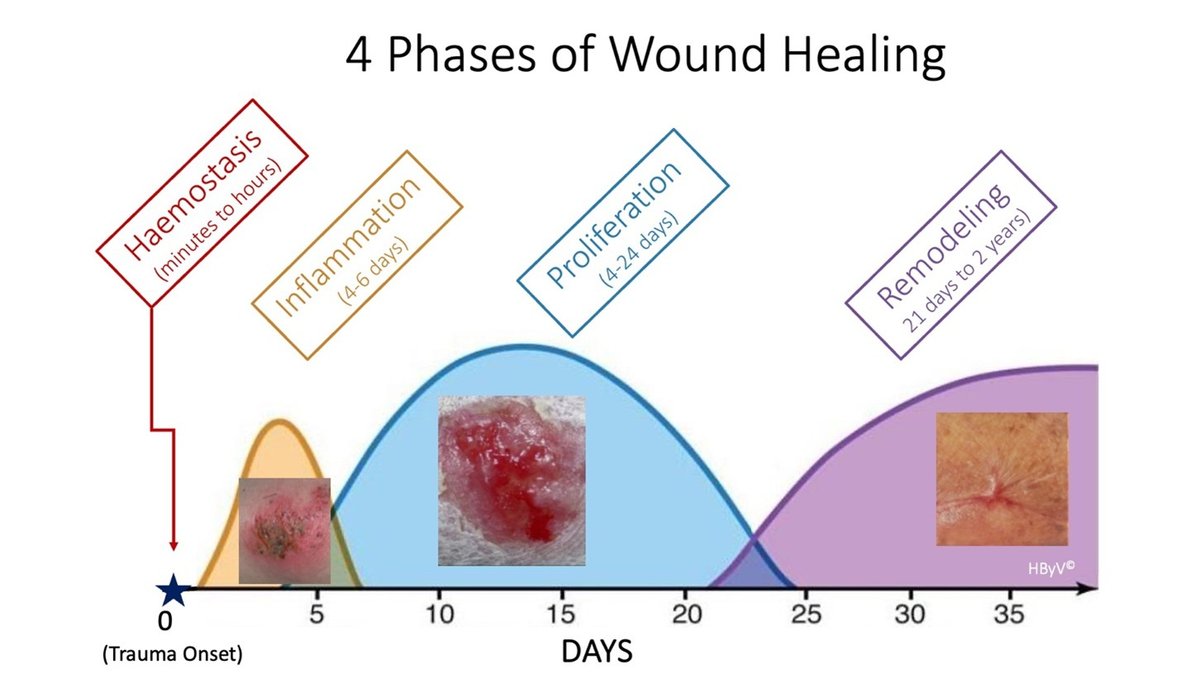
Normal wound healing is described in four overlapping phases (Fig. 2). First, skin damage induces haemostasis. Lasting a few minutes, it limits blood loss but also begins the second phase (inflammatory phase). This phase can last up to 1 week and will allow the body’s white blood cells to clear the wound of cellular debris and bacteria. After this, the third phase called the proliferative phase begins. During the 2–3 weeks of this phase, the body’s builder cells, also known as fibroblasts, will multiply and lay down the extracellular matrix (granulation tissue). This allows surface-making cells called epithelial cells to cover the wound (epithelialization) and close it.10 The final phase is called maturation where the fragile scarring tissue will continue consolidating for months. Retraction can also happen in this phase, leading to disability. Sometimes, wound healing stops in one phase (often inflammation) and this leads to chronic wounds.
The six basic principles of wound management
1) Assess wound cause and other relevant diagnosis
Precise diagnosis of the cause of the wound is key and treating the underlying cause is a first step if applicable. A robust assessment of the wound characteristics directs which management is needed.8,9
The TIME-D model (Table 1) is a useful clinical tool to characterize wounds.11,12 It is based on the tissue’s visual appearance (T), presence of inflammation or infection (I), moisture (exudate) content (M), and nature of the extended edge of the wound (E). The ‘D’ adds a reminder to check for other relevant diagnoses, either additional diseases or factors such as pain, nutritional status, smoking, medication, that can affect wound healing and should be corrected.11
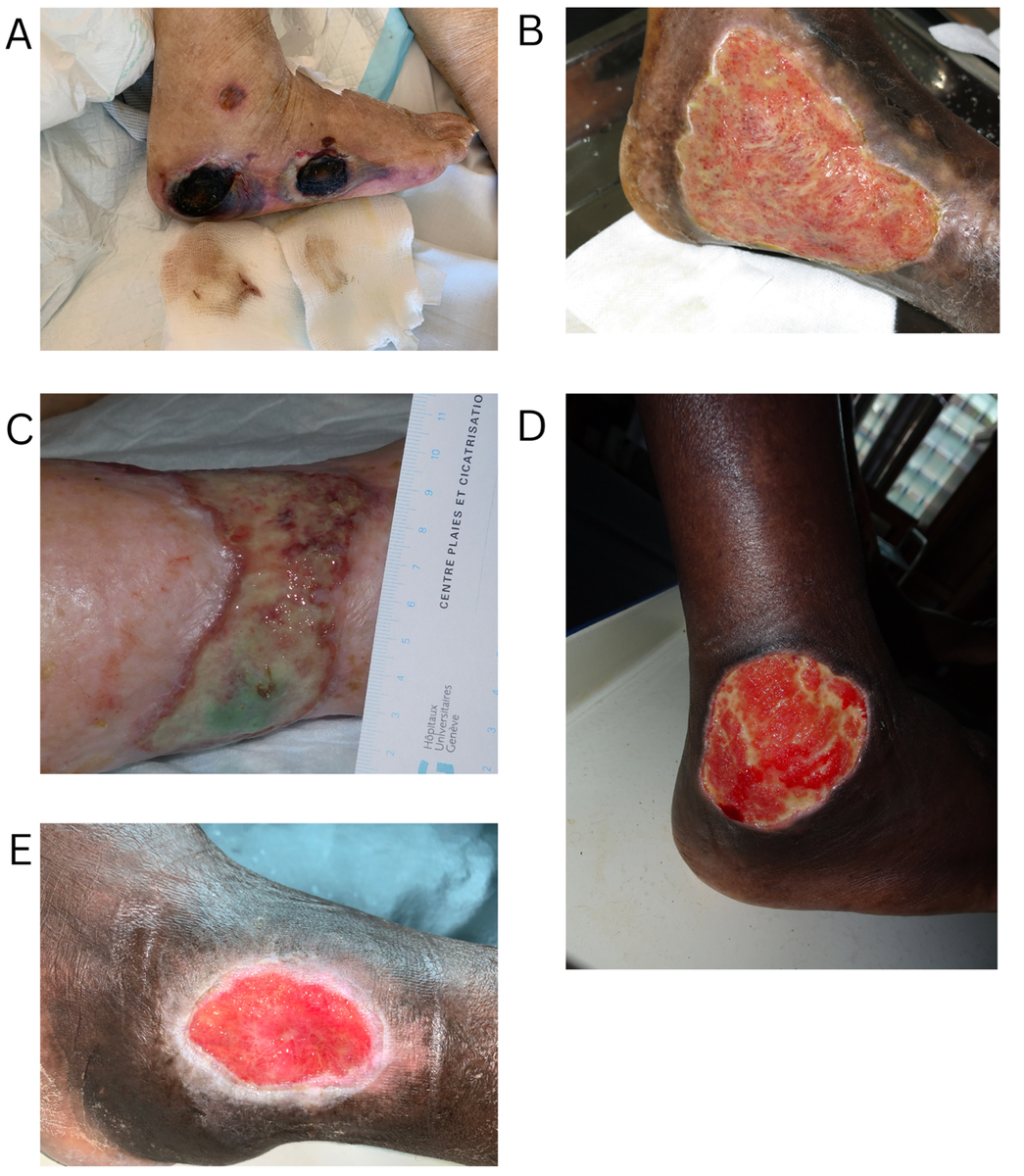
Colour is important to note when assessing tissue. Although not 100% accurate, these colours have become good general standards in describing the wound bed (Fig. 3).
- Black tissue is commonly a sign of necrosis (dead tissue).
- Yellow tissue frequently suggests fibrin deposition, an important protein for initial clotting but of little use in further stages.
- Tissue with necrosis or fibrin will need to be scraped to allow for proper wound healing.
- Green tissue is frequently a sign of infection and will need to be treated with antimicrobials.
- Red tissue is usually a sign of granulation and pink tissue is usually a sign of epithelization.
- Both red and pink tissue suggests that the wound is healing appropriately.
- More than one type of tissue (i.e. more than one colour) can exist in a wound bed at a time.
2) Maintain a controlled moist wound-bed environment
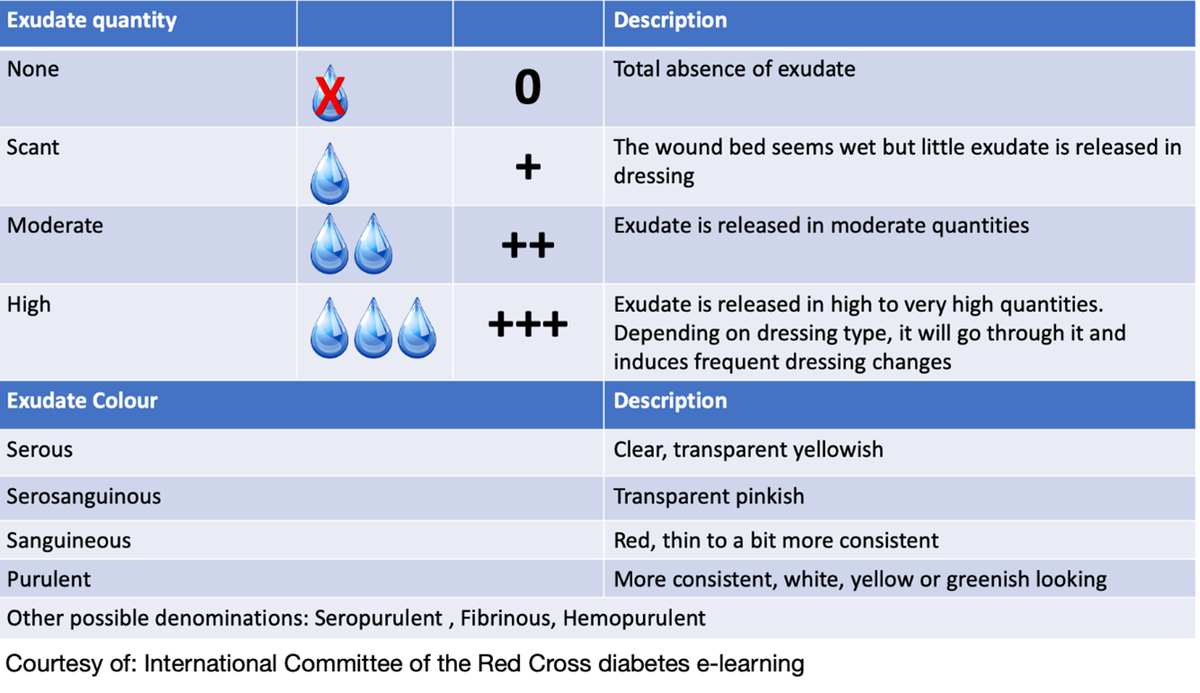
As roughly 70% of the human body is made up of water, it is important for good wound healing to mimic this biological state by maintaining a moist wound bed. A good wound dressing needs to retain necessary moisture yet absorb excess moisture (moisture balance). It will usually also ease pain. Wounds can also produce fluid. This exudate can either be part of the normal healing process or can be a sign of abnormal healing such as poor haemostasis or infection. It is also important to assess the quantity and type of exudate to understand whether the wound is healing well (Fig. 4).
3) Protect wound and peri-wound skin from further trauma
Since wounds are fragile, one must prevent additional damage that may occur to the wound bed or the weakened skin.8 Mechanical damage occurs frequently when dressings stick to the wound and/or adhesive bandages are harshly removed from the skin. Chemical damage can occur when excessive disinfection is used, as many such products, especially if used for too long, can be harmful to the wound bed. Lastly, excessive dryness and coolness can lessen cells’ activity and impair healing. Thus, we recommend using nonstick dressings and soaking them, and adhesives, with saline or potable water before removal (Fig. 5). Use of saline or potable water to clean wounds is preferable; only use disinfectants on locally infected wounds.


6) Promote a clean wound bed and control infection
The wound bed is the foundation for good wound healing; it must be clean and free from infection.8 First, all necrosis and fibrin must be removed through a process known as debridement. Large wounds will need instrumental debridement to remove dead tissues (with scalpel blade, scissors, curette). After removal, the fresh wound bed should be rinsed and cleaned with potable water or saline to clear out excess microbes or debris (Fig. 6).
Water fit for drinking is fit for wound care. In case of clinically proven spreading or general infection, systemic antibiotic therapy is combined with topical antiseptics.13 Because of poor action, resistance risks and sensitization, topical antibiotics are not used routinely now.


5) Control both peri-wound and limb lymphoedema/oedema
Oedema is excess body fluid in any part of the body that leads to swelling (Fig. 7). In wounds, it is the result of excessive inflammation in which fluids leak through blood vessels to tissues and/or destruction of nearby lymphatics that compromises fluid resorption. Oedema caused by primary medical conditions such as heart failure can worsen oedema at the wound level. Saturated with inflammatory components, including proteases and dead white blood cells,
oedema delays wound healing and impairs mobility.8 Whenever possible, limit oedema through physical compression (socks or bandages) and increasing physical activity. Compression should not be used, if the limb arteries are obstructed.
6) Prevent or treat physical sequelae/disability
During the healing process, tissue shrinkage can occur. Shrinkage of large wounds and wounds over joints can lead to significant disability Fig. 8). Active physiotherapy started early can prevent such tissue traction and reduce/prevent resulting disability.8 Involving the patient in understanding exercises and correct positioning during the healing process also minimizes the disability risk.
Conclusion
Chronic wounds are a neglected global health challenge that requires more attention. Understanding basic wound healing principles can help to prevent the development of chronic wounds. This includes assessing for the aetiology of the wound, maintaining a moist wound-bed environment, reducing further trauma to the wound and surrounding skin, keeping the wound clean, limiting oedema and preventing further disability. Minimizing the burden of chronic wounds with simple interventions is achievable in low-resource as well as highly resourced settings. Providing information about basic wound care techniques to all healthcare workers as well as patients and patient families will lead to improved outcomes and reduced healing times.
We encourage the reader to learn more about wound care at OpenWHO (see Wound management in resource-limited settings, In Press).
References
- Sen CK. Human Wound and its burden: updated 2020 compendium of estimates. Adv Wound Care 2021; 10:281–92.
- Lotz ME. The burden of wounds in a resource-constrained tertiary hospital: s cross-sectional study. Wound Heal S Afr 2019; 12:29–33.
- Gupta S, Sagar S, Maheshwari G, Kisaka T et al. Wounds Asia 2021; 4:8–14.
- Oluwatosin, OM. Wound Care Practices and Challenges in Nigeria. Adv Skin Wound Care 2007; 20:375–8.
- Levine JM. Wound care in the 21st century: lessons from ancient Egypt. JAMDA 2000; 1:224–7.
- Guest JF, Fuller GW, Vowden P. Cohort study evaluating the burden of wounds to the UK’s National Health Service in 2017/2018: update from 2012/2013. BMJ Open 2020; 10:e045253
- Olsson M, Järbrink K, Divakar U et al. The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen 2019; 27:114–25.
- Keast DH. Wound and Lymphoedema Management: Focus on Resource-limited Settings, 2nd edn. Frederiksberg, Denmark: World Alliance for Wound & Lymphedema Care, 2020.
- Brooks J. Principles of wound management in resource-poor areas. Community Skin Health 2020; 16:8–10
- Wallace HA, Basehore BM, Zito PM. Wound Healing Phases. Treasure Island, FL: StatPearls Publishing, 2023.
- Marelli A, Calwuaerts A, Wagner E et al. Wound care protocol. Available at: https://www.globalfirstaidcentre.org/wp-content/uploads/2021/03/L029NURM02E-P_Wound-Care-protocol_OCB_EN_2018.pdf (last accessed 20 March 2024).
- Schultz GS, Barillo DJ, Mozingo DW, Chin GA. Wound bed preparation and a brief history of TIME. Int Wound J 2004; 1:19–32.
- Cowling T, Jones S. Topical Antibiotics for Infected Wounds: A Review of the Clinical Effectiveness and Guidelines . Ottawa, ON: Canadian Agency for Drugs and Technologies in Health, 2017.